Lateral (Outer) Hip Pain
Typical Symptoms
Lateral (outer) hip pain can cause difficulty when walking, squatting climbing the stairs or lying on the side at night. Depending on the root cause, there can also be a snapping or clicking sensation from the ITB or a shooting pain from a nerve irritation in the back. Sometimes, the pain can radiate down to the knee or cause pain in other areas around the hip.

What causes it?
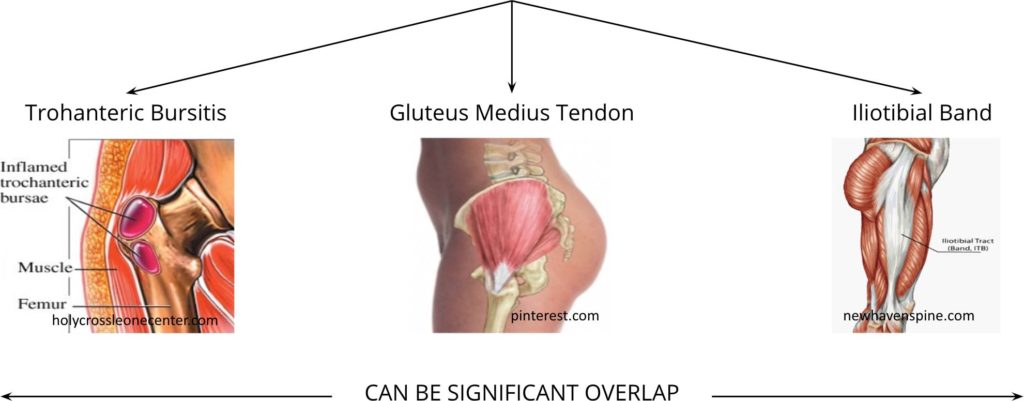
There can be several conditions that can lead to lateral hip pain and these can certainly overlap as well. Common conditions are trochanteric bursitis, gluteus medius tendinopathy and iliotibial band friction.
Symptoms can develop after over-loading of structures on the outside of the hip, from a sudden change in activity, or sometimes a direct impact on to the outside of the hip. It can be made worse with continuing activity or pressure on the area such as lying on the side at night.
How can I help myself?
Consider factors that might have triggered off the symptoms or that continue to aggravate it, such as a change in activity or even a change in footwear. Sleeping on the pain-free side may also help reduce the pressure-related symptoms.
If it is related to particular sporting activities, working with a coach can help or regular soft tissue release with sports therapist can help improve symptoms. Equally, other treatments such as acupuncture or cupping can help relieve tightness symptoms.
When to seek help?
If, despite trying to correct sports technique, movement patterns or soft tissue release, the symptoms are ongoing and it is affecting your sleep or function, you should have your hip pain assessed.
What are the treatment options?
After being assessed with a thorough history and clinical examination, if your clinician suspects that you have developed tightness in the ITB, weakness in or tendinopathy in the gluteus medius tendon or a bursitis, they may undertake investigations such as a hip X-ray (to look for degenerative (wear and tear) changes) or an ultrasound scan (to look for swelling, inflammation or fluid collections). Depending on the problem, they may recommend rehabilitation with a physiotherapist, or a gait analysis and footwear modification with a podiatrist.
If symptoms continue, they might discuss a cortisone or PRP injection to improve your symptoms, but prior to doing this, an MRI may be requested as further investigation. In situations where the is an anatomical injury, a surgical treatment maybe needed.